Background: Invasive aspergillosis (IA) is one of the most dreaded complications in neutropenic patients with hematologic malignancies; risk significantly increases with chemotherapy, particularly during induction. It dramatically worsens the overall prognosis of the underlying malignancy and predisposes patients to undergo secondary interventions, thereby prolonging the duration of treatment and hospital stay. While prophylactic antifungal therapy has remarkably lowered the rates of IA, it remains a persistent problem in cancer treatment. The primary objective of our study is to explore the risk factors of IA in neutropenic patients with acute leukemias and its role in hospital stay, in-hospital mortality, and hospitalization costs.
Methods: The Nationwide Inpatient Sample (NIS) database was queried to include all adults with acute leukemia admitted from 2012 and 2017, whose course was complicated by neutropenia. Those with and without invasive aspergillosis were compared. T-test was used to compare means of continuous variables and chi-square test to compare proportions of categorical variables. Multivariable logistic regression was used to evaluate risk factors for aspergillosis, as well as, inpatient mortality. Statistical tests for trends of resource utilization across six years were performed.
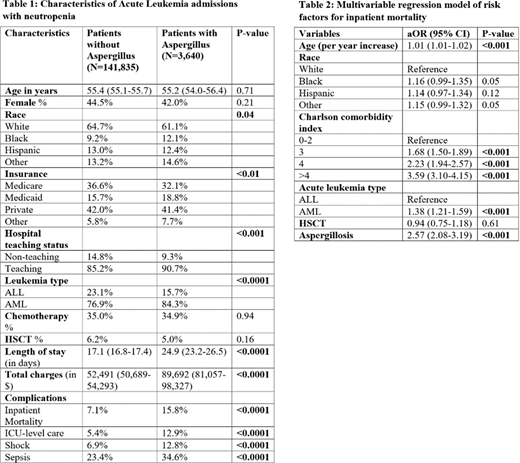
Results: A total of 141,835 admissions met the inclusion criteria, of which, 2.5% had aspergillosis. Mean age (55.4 years) and gender (male 55.5%) did not significantly differ in neutropenic patients with and without aspergillosis. AML accounted for a larger proportion of the aspergillosis group (84.3% vs 76.9%, p<0.0001). Rates of HSCT and inpatient chemotherapy were comparable in both groups. Those with aspergillosis had higher inpatient mortality (15.8% vs 7.1%, p<0.0001) and more frequently required ICU-level care (12.9% vs 5.4%, p<0.0001)
Independent risk factors for the development of aspergillosis included: Black race, receiving treatment at a teaching hospital, AML (compared to ALL) and poor nutritional status. On multivariate analysis, aspergillosis conferred an increased risk of inpatient mortality (aOR 2.57, 95% CI: 2.08-3.19, p<0.001), longer length of hospital stay by 7.4 days (95% CI: 6.0 to 8.8 days, p<0.001) and higher hospitalization costs by $37k per admission (95% CI: $29k-44k, p<0.001).
Rates of aspergillosis decreased from 2.9% in 2012 to 2.2% in 2017 (trend P=0.03). In neutropenic acute leukemia patients without aspergillosis, there has been an improvement in inpatient mortality (from 7.3% in 2012 to 6.0% in 2017, trend P <0.01), as well as, length of hospital stay (17.5 days in 2012 to 16.7 days in 2017, trend P=0.02). However, there was no significant change in mortality or resource utilization among those with aspergillosis.
Conclusions: Aspergillosis represents a significant challenge in the management of hematological malignancies. There is a delicate interplay between neutropenia and IA, with neutropenic patients more susceptible to invasive fungal infections, and IA further contributing to neutropenia. The encouraging trend in decreasing prevalence along the years is reflective of more aggressive prophylactic antifungal usage in acute leukemias, with the revised IDSA guidelines for aspergillosis being a cornerstone. However, mortality and resource utilization remain unchanged despite advances in diagnosis and treatment of aspergillosis. This data highlights the importance of prophylactic antifungals and maintaining a high index of suspicion for IA in neutropenic acute leukemia and the need of early focused treatment to improve clinical outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal